Abstract
Background: Prior studies demonstrated both low and high hemoglobin concentrations are associated with increased mortality. It is unknown whether hemoglobin concentration has a similar U-shaped pattern for coronary heart disease (CHD) risk, or if the relationship differs by age, sex or race.
Objective: We determined the association between hemoglobin concentration and risk of CHD in the national REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort, and addressed whether this association was affected by age, sex, or race.
Methods: REGARDS participants were black and white adults age 45 years and older, enrolled in their homes across the contiguous United States in 2003-7 and followed every 6 months for health outcomes. Baseline risk factors levels were measured using standardized methods, including complete blood counts at a central laboratory, which was initiated after 8608 participants had been recruited. We included REGARDS participants free of CHD at baseline. Incident CHD outcomes were adjudicated by a committee based on medical records review. Cox proportional hazard models were used to examine the association of hemoglobin with incident CHD (both fatal and non-fatal events). Models were adjusted for demographic variables (age, sex, race, and region of residence) and CHD risk factors (hypertension, diabetes, smoking status (current, former, never), total cholesterol (mg/dL), HDL cholesterol (mg/dL), and use of lipid lowering medications). Penalized regression splines were used to graphically represent associations using the adjusted model. Analyses were also stratified by age (≤ 63 vs. > 63), sex (male vs. female), and race (black vs. white).
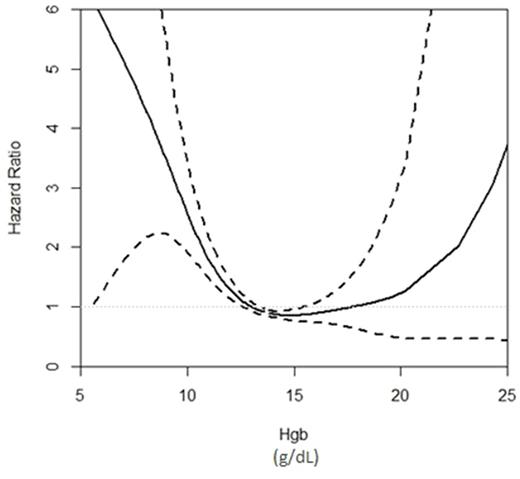
Results: Of 30,239 REGARDS participants, 15,764 had hemoglobin measures, were CHD-free at baseline, and had all baseline variables. The mean age was 63 (IQR 56, 70), 34% were male, and 42% were black. The mean baseline hemoglobin was 13.6 g/dL (SD 1.4). During 118,529 person-years of follow up (median 7.4 years) there were 637 incident CHD events. A significant non-linear association of hemoglobin with CHD was identified after multivariate adjustment (p <0.001). The penalized regression spline graph demonstrated a U-shaped relationship with increasing risk for CHD with lower and higher hemoglobin concentrations, although the confidence intervals were wide (Figure 1). The appearance of age, sex, and race specific regression splines were similar. When hemoglobin was divided into age, sex, and race-specific quintiles, participants in the lowest (HR 1.77; 95% CI 1.38, 2.28) and highest (HR 1.32; 95% CI 1.00, 1.73) quintiles had increased risk of CHD compared to the 4th quintile. The 2nd (HR 1.14; 95% CI 0.86, 1.50) and 3rd quintile (HR 1.22; 95% CI 0.92, 1.60) were not associated with CHD risk.
Conclusion: Hemoglobin concentration was an independent risk factor for CHD, with lower and higher concentrations associated with increased CHD risk. The effect of hemoglobin concentration on CHD risk was a similar shape regardless of age, sex, or race. Further research is needed to explore possible mechanisms mediating the increased CHD risk, but these data point to "optimal" hemoglobin concentrations associated with the lowest CHD risk. Whether hemoglobin concentration is causative or reflects underlying comorbid conditions not accounted for in our analysis requires further work.
Figure 1: Penalized Regression Spline - Hemoglobin Concentration and Hazard Ratio for Coronary Heart Disease
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal